
Product Details
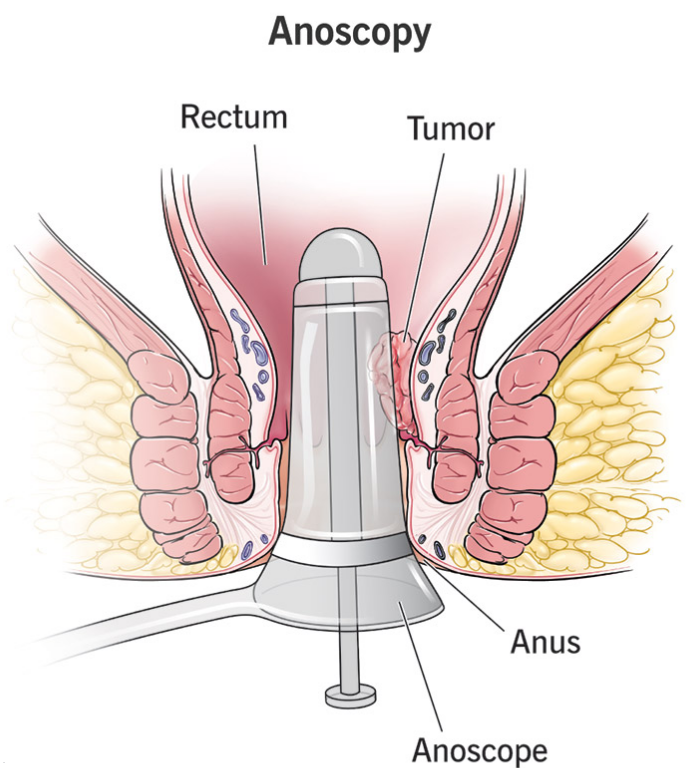
Anoscope: to directly examine the mucosal lining of the distal rectum and anal canal. This procedure enables clinicians to identify structural abnormalities, inflammatory changes, and pathological lesions within the terminal gastrointestinal tract.

Clinical Utility and Comparative Advantages
Superior Sensitivity: Demonstrates higher diagnostic accuracy than flexible sigmoidoscopy for detecting anorectal pathologies including internal hemorrhoids, fissures, fistulae, ulcerations, proctitis, and neoplasms.
Enhanced Visualization: Provides direct assessment of the anal sphincter complex and rectal vault
Primary Diagnostic Indications
Hemorrhoidal Disease: Evaluation of internal/external vascular cushions causing bleeding or discomfort
Anal Fissures: Identification of mucosal lacerations in the anoderm
Inflammatory Conditions: Assessment of proctitis, cryptitis, and perianal dermatitis
Structural Abnormalities: Diagnosis of fistulae, abscesses, and mucosal prolapse
Symptoms Warranting Examination
Rectal bleeding or abnormal discharge
Persistent anal pain/pruritus
Perianal edema or palpable masses
Tenesmus or fecal incontinence
Visible protrusions or tissue irregularities

Procedural Protocol
Insertion of lubricated anoscope beyond the dentate line
Systematic 360° visual inspection during instrument rotation
Selective biopsy/treatment of identified lesions when indicated
HRA Supplementation: Application of acetic acid/Lugol’s solution with colposcopic magnification for enhanced cellular detail
Procedural Characteristics
Duration: 10-30 minutes (extended for HRA or therapeutic interventions)
Risks: Minimal but may include mucosal microtrauma, hemorrhoidal irritation, or transient discomfort
Recovery: Immediate resumption of normal activities; no sedation required

Clinical Significance
Anoscopy remains a fundamental office-based procedure for evaluating distal anorectal disorders. Its capacity for direct visualization, particularly when augmented with high-resolution techniques, provides critical diagnostic information unobtainable through indirect examination methods. The procedure’s rapid execution, minimal invasiveness, and absence of preparatory requirements establish it as an essential tool in proctologic practice.

