Product Details
Arfurla Dual-Wavelength PLDD 980nm 1470nm Spinal Decompression
Minimally Invasive Disc Intervention Device
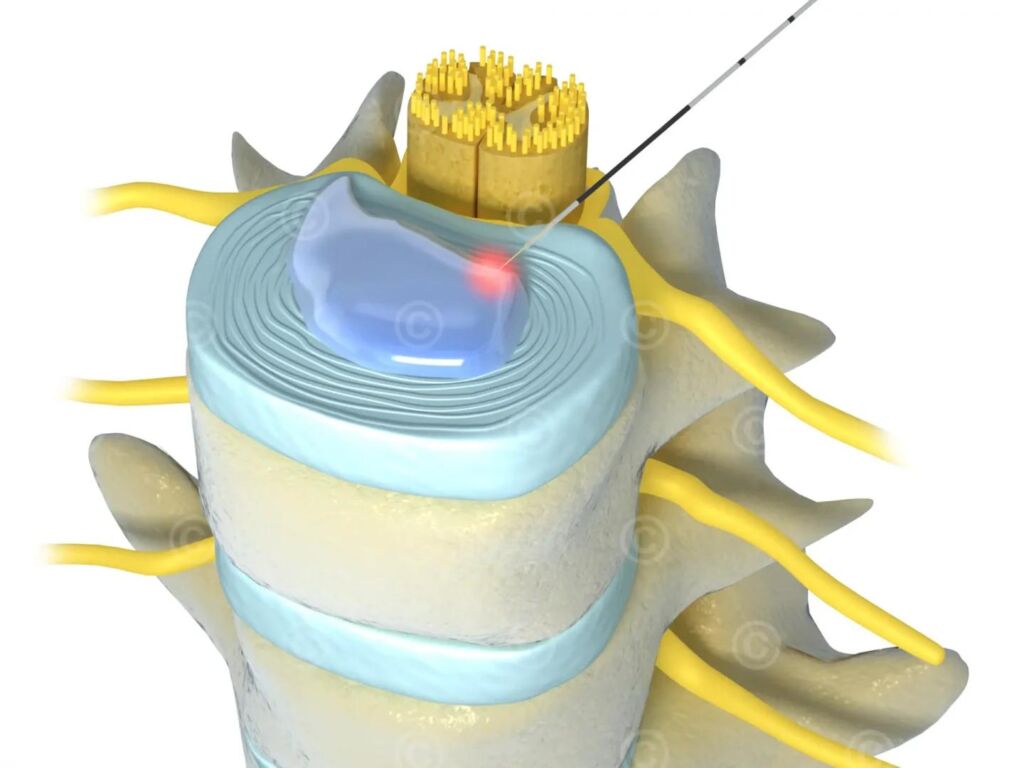
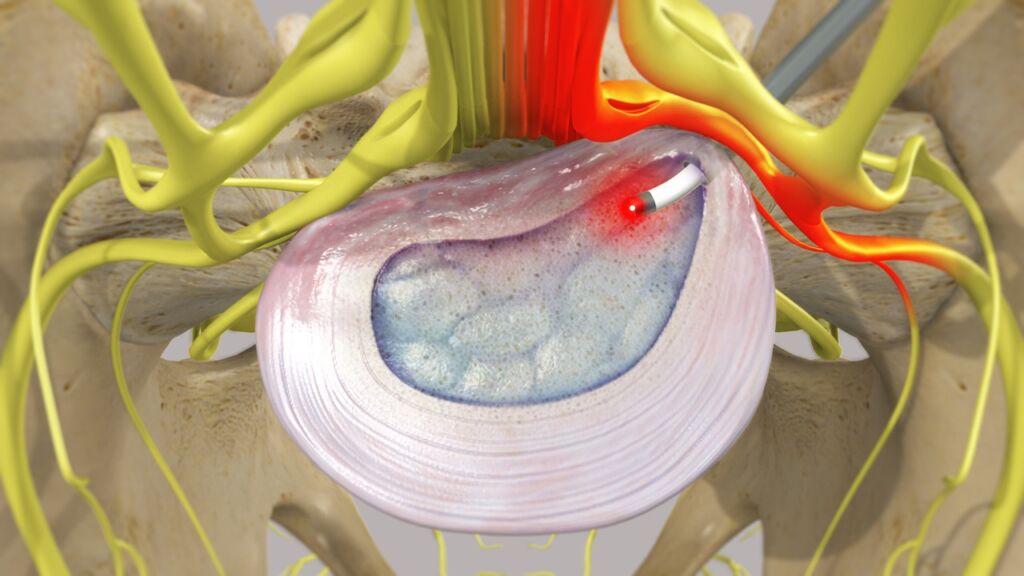
Percutaneous Laser Disc Decompression (PLDD) represents an advanced outpatient procedure for addressing herniated discs across cervical, thoracic (excluding T1-T5), and lumbar regions. This technique employs precisely controlled laser energy delivered via optical fiber to thermally ablate targeted nucleus pulposus tissue. The vaporization of this central disc material creates significant intradiscal pressure reduction, facilitating herniation retraction and consequent symptom relief without open surgery.
Treatment Method | Advantages | Limitations |
PLDD | Minimally invasive, quick recovery, low risk of complications | Not suitable for severe disc herniations or spinal instability |
Open Surgery | Effective for severe cases, direct visualization of the disc | Invasive, longer recovery, higher risk of complications |
Conservative Therapy | Non-invasive, includes physical therapy and medications | Often ineffective for severe or persistent symptoms |
Otology On ENT Laser Surgery Treatment

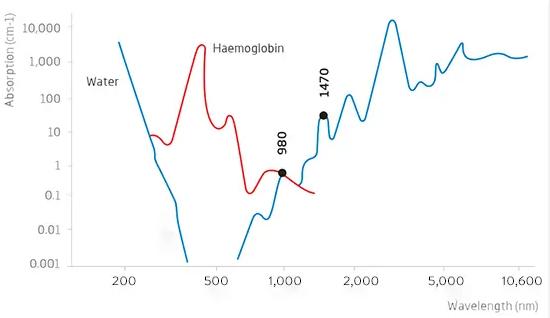
Wavelength-Specific Tissue Interactions:
980nm Laser: Exhibits balanced absorption by hemoglobin and water, enabling effective tissue ablation with inherent hemostatic properties.
1470nm Laser: Features enhanced water absorption characteristics, delivering precise thermal effects with minimal collateral thermal spread. This wavelength
is particularly advantageous near critical neural anatomy due to its controlled penetration depth and optimized safety profile.
Key Clinical Advantages:
Minimal Tissue Trauma: Performed via sub-2mm access point
Local Anesthesia: Eliminates general anesthesia risks
Rapid Procedure: Typically 30-60 minutes completion time
Accelerated Recovery: Most patients resume normal activities within 48-72 hours
Reduced Complication Profile: Lower infection risk versus open procedures
Outpatient Setting: No hospitalization required
Cost Efficiency: Reduced surgical/aftercare expenses
Immediate Symptom Relief: Often experienced intraoperatively
Clinical Indications:
- Contained disc herniations (intact annulus fibrosus)
- Discogenic pain syndromes
- Disc-related spinal stenosis
- Radicular symptoms (sciatica, limb numbness/weakness)
- Chronic back pain refractory to conservative management
Mild-to-moderate herniations without severe neurological compromise

Comparative Treatment Analysis:
PLDD Advantages: Minimally invasive approach, rapid recovery, lower complication rates, cost-effectiveness
PLDD Limitations: Unsuitable for severe herniations, sequestered fragments, or spinal instability
Open Surgery: Reserved for complex cases despite higher morbidity
Conservative Therapies: Often insufficient for mechanical compression pathologies.
Operational Mechanism
- Guided Access:Under real-time imaging (fluoroscopy/CT), a specialized needle accesses the affected disc under local anesthesia.
- Energy Application:Laser energy transmits through an optical fiber into the nucleus pulposus.
- Tissue Ablation:Controlled thermal vaporization of disc material reduces volume and internal pressure.
- Neurological Decompression:Diminished pressure enables herniated disc material to retract from neural structures.
- Vacuum Effect:Creates localized negative pressure drawing herniation away from nerve roots.
Tissue Stabilization: Forms intradiscal scar tissue to prevent recurrence.
Therapeutic Rationale:
PLDD leverages tissue-selective photothermolysis where laser energy:
- Precisely vaporizes nucleus pulposus aqueous content
- Generates immediate intradiscal pressure reduction (typically 35-55%)
- Facilitates retraction of herniated material
- Creates favorable conditions for fibrotic healing
- Preserves disc biomechanical function
Arfurla’s dual-wavelength PLDD device provides a scientifically validated, minimally invasive solution for contained disc pathologies. By achieving targeted decompression through precise thermal ablation, this technique offers significant advantages over traditional surgical options for appropriately selected patients, including reduced tissue trauma, accelerated functional recovery, and lower healthcare costs. The wavelength-specific tissue interactions enable optimized treatment safety and efficacy across cervical, thoracic, and lumbar applications, establishing PLDD as a premier intervention for mechanical radiculopathy management.